 |
|
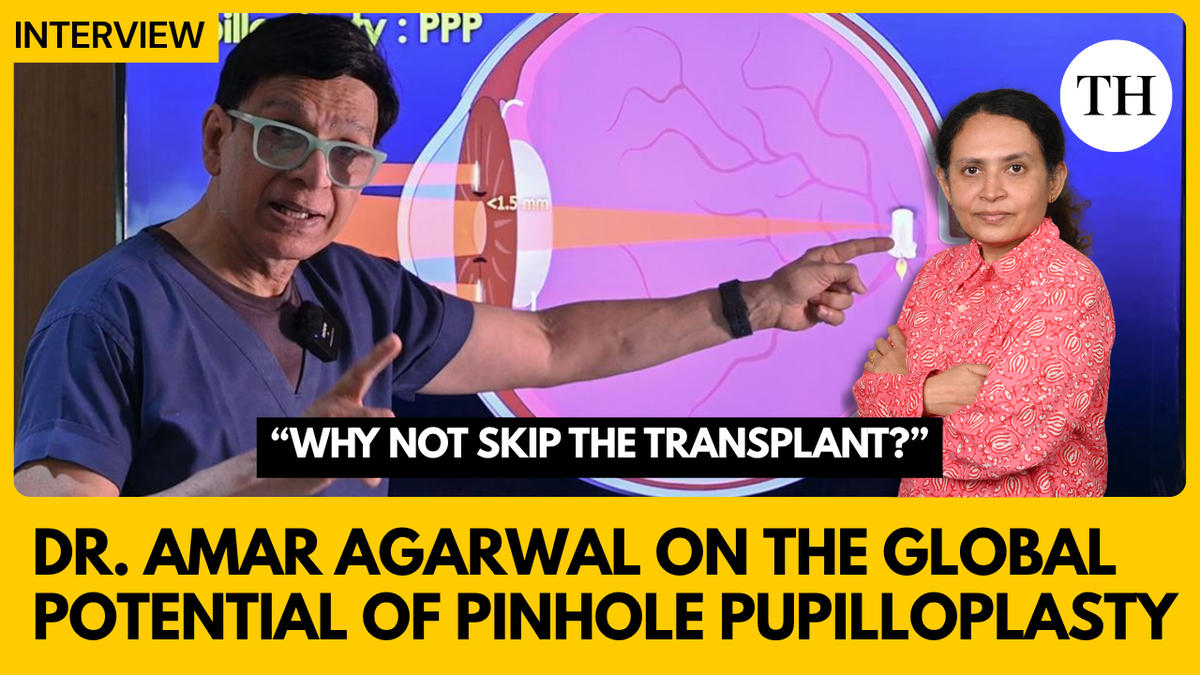
Dr. Amar Agarwal's innovative surgical technique, Pinhole Pupilloplasty (PPP), represents a significant advancement in ophthalmic care, particularly in addressing corneal opacities and visual impairment. This procedure offers a potentially transformative solution for patients who might otherwise require corneal transplants, a complex and often inaccessible treatment, especially in resource-limited settings. The core principle behind PPP lies in creating a small, centrally located aperture in the iris, effectively functioning as a pinhole camera. This pinhole effect increases the depth of focus, thereby improving visual acuity even in the presence of corneal irregularities or opacities. The article highlights the potential of PPP to provide near 20/20 vision for patients post-surgery, a remarkable outcome that significantly enhances their quality of life. One of the most compelling aspects of PPP is its relative simplicity and accessibility. Dr. Agarwal emphasizes that any trained eye surgeon can perform the procedure, making it a readily deployable solution in diverse healthcare environments. This contrasts sharply with the specialized expertise and infrastructure required for corneal transplantation, which often limits its availability to patients in developing countries or remote areas. Furthermore, PPP is presented as a low-cost and low-risk alternative to corneal transplants. The reduced financial burden associated with PPP makes it a more equitable option for patients who may not be able to afford the considerable expenses of transplantation, including surgery, donor tissue acquisition, and post-operative care. The lower risk profile of PPP, compared to the potential complications of transplant rejection or infection, further enhances its appeal as a first-line treatment strategy. The interview with Dr. Agarwal underscores the global potential of PPP to alleviate the burden on the world’s corneal transplant system. By providing a viable alternative for a significant proportion of patients with corneal opacities, PPP could free up transplant resources for those with more severe or irreversible corneal damage. This shift in treatment paradigm could lead to more efficient allocation of healthcare resources and improved visual outcomes for a larger population of patients. The success stories attributed to PPP, with patients achieving near 20/20 vision, serve as powerful testimonials to its efficacy and impact. These anecdotal accounts provide tangible evidence of the transformative effect of the procedure on individual lives, inspiring hope and encouraging wider adoption of PPP within the ophthalmic community. The potential of PPP extends beyond its direct impact on visual acuity. By restoring vision, the procedure can empower patients to regain independence, participate more fully in daily activities, and contribute more effectively to their communities. The psychological and social benefits of improved vision are often overlooked but are crucial determinants of overall well-being. PPP's impact on these aspects of life further solidifies its value as a healthcare innovation. The global uptake of PPP, as discussed in the article, reflects its growing recognition and acceptance among eye surgeons worldwide. The simplicity of the procedure, coupled with its proven efficacy and low risk profile, has contributed to its rapid adoption in various clinical settings. This widespread dissemination of PPP is a testament to its potential to address a significant unmet need in ophthalmic care and to improve the lives of countless individuals suffering from corneal opacities. In summary, Pinhole Pupilloplasty represents a paradigm shift in the management of corneal opacities. Its simplicity, accessibility, low cost, and low risk profile make it a compelling alternative to corneal transplantation, with the potential to improve visual outcomes for a large population of patients worldwide. The global uptake of PPP underscores its growing recognition as a valuable tool in the ophthalmic armamentarium and its potential to alleviate the burden on the world’s corneal transplant system.
The interview format allows Dr. Agarwal to directly communicate the advantages of PPP. He positions PPP not just as a surgical alternative, but as a more accessible and practical solution, especially in regions where corneal transplants are scarce or financially prohibitive. This direct communication strategy is effective in conveying the message that PPP is not a replacement for corneal transplants in all cases, but a valuable tool to manage certain types of corneal opacities, reducing the immediate need for more complex and resource-intensive procedures. The emphasis on the ease of learning and implementation is crucial. By stating that any eye surgeon with some training can perform PPP, Dr. Agarwal addresses a key barrier to adoption. It implies that widespread implementation is achievable without requiring extensive specialization or investment in new equipment. This accessibility is a major factor in PPP's potential global impact, allowing more surgeons to offer this treatment option to their patients. The mention of 'near 20/20 vision' is a powerful and attention-grabbing statement. It provides a concrete and easily understandable measure of success, further reinforcing the potential benefits of PPP. While the article doesn't delve into the specifics of patient selection, this statement sets a high expectation for visual outcomes and is likely to resonate with both patients and clinicians. The article's structure, focusing on an interview with the innovator, lends credibility and authority to the claims made. Dr. Agarwal's position as chairman of Dr. Agarwal's Eye Hospitals further reinforces his expertise and experience in the field. This positioning enhances the trustworthiness of the information presented and encourages greater acceptance of PPP as a viable treatment option. Furthermore, the presentation and editing credits acknowledge the contributions of the team involved in producing the article. This transparency adds to the overall professionalism and credibility of the piece. By attributing the work to specific individuals, it emphasizes the collaborative effort behind the dissemination of information about PPP and reinforces the commitment to quality and accuracy. The title, “Why not skip the transplant?” is provocative and effectively captures the core message of the article. It directly challenges the conventional approach to treating corneal opacities and invites readers to consider PPP as a potentially superior alternative. This engaging title is likely to draw attention and generate interest in learning more about the procedure. Finally, it's important to acknowledge the potential limitations of the article. As an interview with the innovator of PPP, it is likely to present a favorable view of the procedure. While the article highlights the benefits of PPP, it may not fully address the potential risks, complications, or limitations. A more balanced perspective would require independent research and analysis from other experts in the field.
A critical assessment of Pinhole Pupilloplasty necessitates exploring its limitations and potential drawbacks, which are not extensively covered in the provided article. While presented as a revolutionary alternative to corneal transplantation, PPP might not be universally applicable to all cases of corneal opacity or visual impairment. The specific indications for PPP and the ideal patient profile need careful delineation to ensure optimal outcomes and avoid inappropriate use. For instance, patients with severe corneal scarring, significant irregularities in corneal topography, or underlying retinal pathologies might not benefit substantially from PPP. A thorough preoperative evaluation, including detailed corneal topography, wavefront analysis, and retinal examination, is crucial to determine the suitability of PPP for each individual patient. Furthermore, the long-term efficacy and stability of PPP remain to be fully established. While the article mentions near 20/20 vision post-surgery, longitudinal studies are needed to assess the durability of these visual improvements over time. Factors such as progressive corneal changes, iris atrophy, or pupil distortion could potentially compromise the long-term success of PPP. Regular follow-up examinations and monitoring are essential to detect and manage any potential complications or regressions. Another important consideration is the potential impact of PPP on other ophthalmic procedures. The altered pupil size and shape could potentially affect the accuracy of refractive measurements, cataract surgery, or glaucoma management. Surgeons need to be aware of these potential interactions and adjust their techniques accordingly to avoid adverse outcomes. The creation of a small pupil can also reduce retinal illumination, which could potentially impact vision in dim light conditions or in patients with pre-existing retinal diseases. The article highlights the simplicity of PPP and its accessibility to any trained eye surgeon. However, it is crucial to emphasize the importance of proper training and technique to ensure successful outcomes and minimize complications. Inadequate surgical skills or improper patient selection could lead to suboptimal results or even adverse events, such as iris damage, inflammation, or infection. A standardized training curriculum and mentorship programs are essential to ensure that surgeons are adequately prepared to perform PPP safely and effectively. While PPP offers a potentially cost-effective alternative to corneal transplantation, a comprehensive cost-benefit analysis is needed to fully assess its economic impact. This analysis should consider the costs of the procedure itself, as well as the potential savings in terms of reduced need for corneal transplants, fewer complications, and improved patient outcomes. The availability of PPP could potentially reduce the waiting lists for corneal transplants and improve access to vision-restoring surgery for a larger population of patients. Finally, it is important to recognize that PPP is not a replacement for corneal transplantation in all cases. Corneal transplantation remains the gold standard for treating severe corneal diseases or injuries that cannot be adequately addressed by PPP. The choice between PPP and corneal transplantation should be based on a careful assessment of the individual patient's condition, the severity of their corneal disease, and the potential benefits and risks of each procedure. In conclusion, while Pinhole Pupilloplasty holds significant promise as an innovative and accessible solution for managing corneal opacities, a thorough understanding of its limitations, potential drawbacks, and long-term outcomes is crucial for its responsible and effective implementation. Further research, standardized training, and careful patient selection are essential to maximize the benefits of PPP and ensure optimal visual outcomes for patients.
Source: “Why not skip the transplant?”: Dr. Amar Agarwal on the global potential of Pinhole Pupilloplasty
